Growing and converging evidence suggests that the motor system becomes integrated with the complex processing of nociceptive signals. In patients with amputated limbs, part of the primary motor cortex becomes redundant for its prior tasks, while also being deprived of the sensory feedback. When a critical role of the motor cortex, that of suppressing excessive sensory input into the thalamus and inducing descending pain modulation, is compromised, spontaneous pain may result.
Finnish rTMS patient case
Hear first hand from a patient in the Helsinki University Hospital & Orton pain treatment program, how navigated rTMS changed his live (subtitles are available in English).
rTMS offers a truly significant analgesic effect
In patients with neuropathic pain, evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation* make a Level A recommendation for the truly significant analgesic effect of high-frequency rTMS targeted at the motor cortex, contralaterally to the pain side. Tolerance of rTMS is rated as excellent, even in patients with chronic refractory pain.
rTMS has shown better efficacy in patients with neuropathic pain of cortical or peripheral origin than in patients with lesions affecting the brainstem or the spinal cord.
Target site selection
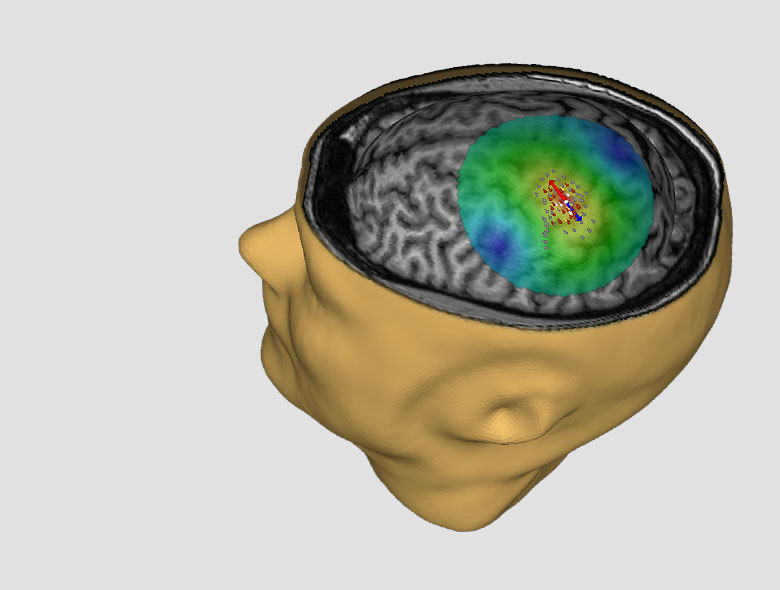
Experts agree that image-guidance of the therapy — the NBS 6 with SmartFocus® nTMS — is required, since determining the exact stimulation site within the motor cortex is critical for obtaining the optimal therapeutic response. Cortical reorganization can add an additional challenge in selecting a site for targeting the stimulation and numerous studies have shown evidence of more pronounced analgesic effects when the region adjacent to the painful region is targeted with rTMS.
In chronic pain there is significant cortical reorganization within the primary motor cortex and the corticomotor maps are in a state of flux. rTMS treatment can normalize the representation area of the primary motor cortex and have a therapeutic effect—patients who do not respond to rTMS therapy have not shown normalization in the motor cortex.
Stimulation parameters and durability
The analgesic effects of rTMS depend on the frequency of stimulation. When targeted to the motor cortex contralateral to the painful side at frequencies of 5 Hz, or higher, rTMS relieves pain. The analgesic effects of rTMS are related to the excitation of neural circuits lying in the superficial layers of the cortex, tangential to the surface of the precentral gyrus.
High frequency rTMS increases cortical excitability beyond the time of stimulation. The maximal analgesic effect of a single session of rTMS occurs after 2–3 days and may extend for up to one week. In fibromyalgia, it has been shown that pain control can be maintained for up to six months by monthly rTMS treatments, following an induction phase of daily 20-min rTMS sessions for 5 days.
Nexstim Protocol (CE mark)
In patients suffering from unilateral chronic neuropathic pain, the motor representation area corresponding to the pain location on the hemisphere contralateral to pain is enlarged (Nurmikko et al.). With Nexstim NBT the specific cortical targets for rTMS delivery are obtained by bilateral motor cortex mapping of both hemispheres and comparing the motor representation areas to each other. The primary therapy target is chosen as the hotspot of muscle representation area of the muscle corresponding to the location of pain (for hand pain – First Dorsal Interosseus muscle, for leg pain – m.Tibialis Anterior, for facial pain – m.Orbicularis Oris) that also resides within the mirror image of the same motor representation area on the unlesioned hemisphere. After the target is localized, the Nexstim NBT System is used to determine the patient’s individual MT of the target location. With the stimulator output set to up to 100% intensity of individual MT, the rTMS therapy (10 Hz, 20 trains of 100 pulses, total of 2000 pulses) is then started. If, after 2-3 treatment sessions no response is obtained, stimulation of a second therapy target - the motor cortex hotspot of the muscle representation area contralateral to the pain that is outside the corresponding representation area of the same muscle on the unaffected hemisphere may result in clinical benefit (see below).
Pre-surgical rTMS therapy in MCS implantation
Although epidural MCS can be an effective method to treat drug-resistant neuropathic pain, the procedure is invasive and there are no reliable preoperative criteria to predict outcome.
As a non-invasive technology, rTMS can play a role in identifying responders to MCS pre-surgically. Patients who respond to rTMS respond to MCS with an extremely high positive predictive value, although rTMS has a low predictive value to rule patients out from surgery. A positive response to rTMS therapy can help patients accept epidural implantation.
The validation of a cortical target by preoperative rTMS helps neurosurgeons plan and optimize epidural electrode placement in MCS implantation.
Interested in a live demo of nTMS?
Our team of physicians, researchers, and engineers is prepared to answer your questions. If you would like to learn more or set up a virtual demonstration for your team, please contact us!
Yes, I would like to know more
Indications for use (CE mark) and patient safety
Nexstim NBS 6 is not approved by the Food and Drug Administration for commercial use of the treatment of chronic pain in the United States, for investigational use only.
CE mark Intended use
Nexstim NBS 6 for depression is intended to be used for treatment of major depressive disorder (MDD) by targeting and delivering non-invasive repetitive TMS stimulation to the patient's dorsolateral prefrontal cortex.
CE mark Indications for use
Nexstim NBS 6 is indicated for MRI-guided and electric field (or E-field) navigated, non-invasive, repetitive TMS stimulation (rTMS) of the motor cortex as therapy to alleviate chronic unilateral neuropathic pain in adult patients. Nexstim NBS 6 is intended to be used by trained clinical professionals.
SAFETY
NBS 6 THERAPY SHOULD NOT BE GIVEN TO
- Patients with non-removable conductive, ferromagnetic, or other magnetic-sensitive metal anywhere in the head or within 30 cm (12 in) of the stimulation coil. Examples include cochlear implants, implanted electrodes or stimulators, aneurysm clips or coils, stents, bullet fragments, ocular implants, and stents.
- Patients who have an active or inactive implanted device (including device leads), including deep brain stimulators, cochlear implants, cardiac pacemakers, and vagus nerve stimulators. Contraindicated use could result in serious injury or death.
- Patients with increased intracranial pressure or patients with intracardiac lines, intravenous pumps, or dose calculators.
Failure to follow these restrictions could result in serious injury or death.
RISKS AND SIDE EFFECTS
Seizures (Convulsions): Cortical magnetic stimulation runs the risk of inducing seizures; although they are rare.
The most common side effects reported during clinical studies (Lefaucheur et al., Nurmikko et al.) are: mild headache (25% of the TMS treatment group), sleepiness (38 %), and dizziness (15 %).
No severe adverse events were reported. Specifically, no seizures occurred.
In some patients with chronic neuropathic pain, the pain may transiently worsen after rTMS stimulation. The increase in pain sensation may last up to 1-2 days.
No adverse effects on hearing have occurred when ear protection has been properly worn.
No effects on cognitive function has been reported.
Clinical studies have reported no deaths in rTMS therapy. (Nurmikko et al.)
References
*Lefaucheur JP et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014 Nov;125(11):2150-206. https://www.ncbi.nlm.nih.gov/pubmed/25034472
Nurmikko T et al. Motor Cortex Reorganization and Repetitive Transcranial Magnetic Stimulation for Pain-A Methodological Study. Neuromodulation. 2016 Oct;19(7):669-678. https://www.ncbi.nlm.nih.gov/pubmed/27187056
Other
Ahdab R, Lefaucheur JP 2nd International Symposium on Navigated Brain Stimulation in Neurosurgery Charité - Universitätsmedizin Berlin (Organizer) 2011 May; 34-36
Mylius V, Lefaucheur JP 3rd International Symposium on Navigated Brain Stimulation in Neurosurgery Charité - Universitätsmedizin Berlin (Organizer) 2012 May; 27-29
Nurmikko TJ, Sacco P 3rd International Symposium on Navigated Brain Stimulation in Neurosurgery Charité - Universitätsmedizin Berlin (Organizer) 2012 May; 23-26
Nurmikko TJ, Sacco P 5th International Symposium on Navigated Brain Stimulation in Neurosurgery Charité - Universitätsmedizin Berlin (Organizer) 2014 June; 32-36
Nurmikko T et al. Motor Cortex Reorganization and Repetitive Transcranial Magnetic Stimulation for Pain-A Methodological Study. Neuromodulation. 2016 Oct;19(7):669-678.